70 year old male with altered sensorium
N.Deepa, 8th semester
Roll no. 93
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Following is the view of my case : ( history as per the date of admission 9/10/21 )
CASE :
A 70 year old male patient was bought to the casuality with chief complaints of altered sensorium.
HISTORY OF PRESENT ILLNESS :
Patient was apparently asymptomatic a day before. On 8/10/21 5-6 pm he was absolutely normal and had his dinner around 7pm . Later he felt uneasiness and took a tablet GLIMI. Around 8 pm he couldn't recognize his family members, he had a staring look and gurgling sound. He had a history of fall during this episode. Later the attendees took him to local rmp where he diagnosed him with low sugar levels ( hypoglycemia) . The rmp adminstered iv fluids and gave sugar water orally. The patient became absolutely normal later. After observation for some time they went back home at 11 pm. At 4 am in the morning the attendees found that the patient had similar episode as previous and the rmp referred to our hospital.
PAST HISTORY :
Patient is a known case of hypertension since 1 year and diabetes since 1 month.
For hypertension - tab. TELMA 40 mg OD
For diabetes - tab. GLIMI OD
FAMILY HISTORY :
No significant family history.
PERSONAL HISTORY :
Diet - Mixed diet
Appetite - Normal
Sleep - Adequate
Bowel and bladder movements - Regular
Allergies - No food and drug allergies
Addictions - alcohol occasionally
GENERAL EXAMINATION :
On 9/10/21 when I examined
The patient was conscious, coherent and co - operative.
He is well oriented to time, place and person.
No pallor
No icterus
No clubbing
No cyanosis
No generalized lymphadenopathy
No bilateral pedal edema
VITALS :
Temperature : Afebrile
Pulse : 100 bpm
Blood pressure : 100/60 mm of hg
Respiratory rate : 20 cycles / min
Spo2 : 95%
SYSTEMIC EXAMINATION :
Cvs : S1 S2 heart sounds heard, No murmurs
Respiratory system : Bilateral air entry present.
Cns : Intact
Patient was aphasic at the time of presentation.
When I was examined he regained his speech.
Abdomen : Soft and non - tender. Bowel sounds are heard. No organomegaly.
INVESTIGATIONS :
Usg : raised echogenicity of kidneys on both sides
DIAGNOSIS :
Altered sensorium secondary to hypoglycemia secondary to oral hypoglycemic agents.
TREATMENT :
On 9/10/21 :
• Nil by mouth
• Stop oral hypoglycemics and other anti hypertensive drugs
• Inj. PAN 40 mg IV /OD
• IVF Normal saline 75 ml /hr
• GRBS monitoring
• IVF - 5% dextrose 75 ml / hr
If GRBS < 100 mg/dl
• Strict I/ O monitoring
• Inj. Optineuron 1 amp. in 100ml of normal saline / IV / OD
• Strict BP, PR monitoring 4rth hourly
On 10/10/21 :
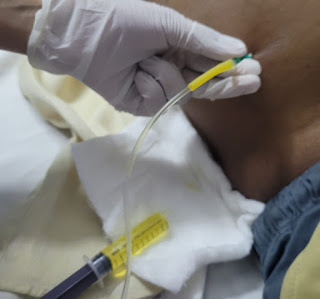
• RT feeds with 100 ml milk with 2 table spoon of sugar with 100ml water
• IVF 25% dextrose 5 ml / hr
( increase or decrease according to GRBS)
• Inj. PAN 40 mg / IV / OD
•Strict I/ O monitoring
• Inj. Optineuron 1 amp. in 100ml of normal saline / IV / OD ( over 30 min)
• GRBS monitoring hourly
• Tab. NODOSIL 500 mg RT/ OD
• Tab. AMLONG RT/ OD
• Tab. SHELCAL RT / OD
On 11/ 10 / 21 :
• Inj. PAN 40 mg / IV / OD
• Inj. Optineuron 1 amp. in 100ml of normal saline / IV / OD ( over 30 min)
• Tab. NODOSIL 500 mg RT/ OD
• Tab. AMLONG RT/ OD
• Tab. SHELCAL RT / OD
• Inj. HAI s/c according to GRBS
8am - 2pm - 8pm
On 12/10/21 :
GRBS was 190 .
Patient is kept on insulin.
Patient got discharged.





Comments
Post a Comment