65 year old female with difficulty in swallowing
N.Deepa, 9th semester
A 65 year old female, herder by occupation, bought to the opd with chief complaints of
~Ear pain and ringing sensation in ears on and off since 2 years
~Generalised weakness since 1year
~Pain of right fingertips since 2 months
~Dryness of mouth and inability to swallow since 2 months
• Dryness of mouth since 2 months associated with difficulty in swallowing. It was insidious in onset and gradually progressive. The difficulty in swallowing is more for solids than liquids. She apparently can only swallow if she drinks water along with her food. It is associated with loss of appetite and early satiety. She feels like her voice has also changed as she feels pain on trying to talk.
• Pricking type of Pain of right fingertips since 2 months, which is constant, increases on activity such as mixing food or combing hair so she stopped doing house chores and sleeps most of the time.
There is discoloration at the tips of fingers.
•2 months back, after getting down the bus, she landed on a sloped surface, lost her balance and tumbled down. She lost her consciousness for 5 minutes and was later woken up by her daughter and was given water. She walked back home after this episode. She had trauma to head and laceration on her left arm.
•She has history of fall on 28/3/22 at 8pm when she went to take a bath, she sat on a stool and fell back.
•At 3 AM, she woke up to urinate, went to the washroom and sat in squatting position, before she could support herself with her hands she fell on her face and that resulted in a swollen right eye.
VITALS:
PR: 90bpm
BP: 110/70mmHg
RR: 16cpm
Temperature: Afebrile
SYSTEMIC EXAMINATION :
CVS: S1 S2 present
No murmurs, thrills heard.
RS: BAE present, NVBS heard.
CNS: E4V5M6
HMF: intact. Conscious.
Tone: R. L
UL. N. N
LL. N. N
Power: R. L
UL. 5/5. 5/5
LL. 5/5. 5/5
Rhomberg sign - negative
Gait :
Investigations:
RBS: 164 mg/dl
Se. Creatinine: 1.2 mg/dL( on 29/3/2022)
2.4mg /dL ( on 28/3/2022)
Se. Uric acid: 11.1 mg/dL
Blood urea: 41 mg/dL
Na: 138 mEq/L
K: 4.8 mEq/L
Cl: 101 mEq/L
LFT:
Db: 0.16 mg/dL
Tb: 0.57 mg/dL
AST: 64 IU/L
ALT: 57 IU/L
ALP: 204 IU/L
TP: 8.0 gm/dL
Albumin: 3.6 gm/dL
A/G ratio: 0.89
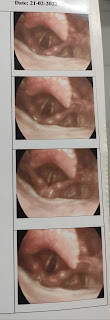
Direct laryngoscopy
( done in other hospital before admission)
Doppler 2d echo:
X- rays :
Provisional Diagnosis:
Crest syndrome?
Heart failure?
Sensory ataxia?
Treatment plan:
1. Tab. NIFEDIPINE 10mg TID
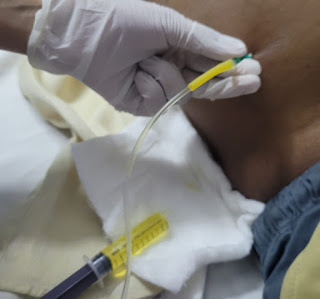
2. IV FLUIDS 2 NS
3. Inj. ACTRAPID 10 units
(Morning- afternoon-night)
4. Tab. FOLITRAX ( methotrexate)7.5mg once a week
Every Wednesday
5. Tab.FOLIC ACID 5mg once a week on Tuesday.
































Comments
Post a Comment