60 year old female with history of SOB
N.Deepa, 8th semester
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Following is the view of my case : (Admitted on 12/05/21 , 11 am)
CASE :
60 year old female came with the chief complaints of SOB since 2 days, cough since 2 days and giddiness since morning 6 am.
HISTORY OF PRESENT ILLNESS :
Patient was apparently asymptomatic 2 days back. Then she developed SOB which is of sudden in onset and progressive in nature. SOB is not associated with chest pain, palpitations, sweating, nausea, vomiting, blackouts, blurring of vision, Trauma to chest.
She also has cough since 2 days. It is associated with sputum in small quantity. Patient attenders denied the history of fever, cold, sore throat, vomiting, loose motions, headache.
Giddiness is sudden in onset and there is no change with change of position.
PAST HISTORY :
Patient is a known case of diabetes mellitus type -2 since 5 years. No history of hypertension, epilepsy, tuberculosis, CVA, CAD.
PERSONAL HISTORY :
Diet - mixed
Appetite - decreased
Bowel and bladder habits - regular
Sleep - inadequate
GENERAL EXAMINATION :
Patient was conscious with glass gow coma scale of 11.
GCS
Eye opening - 4 Verbal response - 1 Movement - 6
No pallor
No Icterus
No Cyanosis
No Clubbing
No Generalized lymphadenopathy
No Bilateral pedal edema
VITALS :
Temperature : Afebrile
Pulse : 82 bpm
Respiratory rate : 32 cpm
Blood pressure : 120/90 mm of hg
Spo2 : 60% at room air
88% with 5 litres of oxygen
SYSTEMIC EXAMINATION :
Cvs - S1 S2 heart sounds heard, No murmurs heard
Respiratory system - Bilateral course crepitus in all areas heard
INVESTIGATIONS :
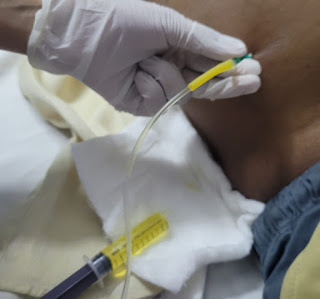
1) Arterial blood gas ( ABG)
PH - 7.42
PCo2 - 25.4 mm hg
PO2 - 39.1 mm hg
HCo3 - 16.1 mmol / lit
St. HCo3 - 18.6 mmol / lit
O2 saturation - 70.5 %
O2 Count - 11.5 vol%



Comments
Post a Comment