Online blended bimonthly assignment toward summative assessment for the month of May 2021
I have been given the following cases to solve in an attempt to understand the topic of 'Patient clinical data analysis' to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and diagnosis and come up with a treatment plan.
This is the link of the questions asked regarding the cases :
Below are my answers to the Medicine Assignment based on my comprehension of the cases.
PULMONOLOGY
CASE 1
A 55 Year Old Female with Shortness of Breath, pedal Edema and Facial Puffiness.
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans : Evolution of symptomatology and Event timeline-
- 20 Years ago - SOB Grade1 for a week , occurred every year for the same duration.
- 12 Years ago - SOB Grade 1 for a month
- 8 Years ago- Polyuria and was diagnosed with DM
- 1 Month ago - Weakness was giving IV
- 30 Days ago - SOB ( latest episode) gradually progressive
- 20 Days ago - HRCT showed Bronchiectasis
- 20 days ago - diagnosed with hypertension
- 15 Days ago - Pedal edema and facial puffiness
- 2 Days ago - SOB Grade 4 , drowsiness and decreased urine output.
Anatomical location of the problem is BRONCHIOLES.
Primary etiology is rice dust exposure as patient is a farmer working in paddy fields.
It can also be due to use of chulha since many years.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Ans :
Head end elevation
• Elevation of head of the bed to 30° improves jugular venous outflow and lowers intra cranial pressure.
• Head elevation by 20°- 40° has been shown to improve oxygenation.
Indications :
• Head injury
• Meningitis
• O2 inhalation to maintain spo2
• Pneumonia
BiPAP stands for Bilevel positive airway pressure. It is a type of now invasive ventilation.
Indications :
- Chronic obstructive pulmonary disorder (COPD)
- Obstructive sleep apnea.
- Obesity hypoventilation syndrome.
- Pneumonia.
- Asthma flare-up.
- Poor breathing after an operation.
- Neurological disease that disturbs breathing.
Augmentin - Amoxicillin + Clavulanic acid.
On each occasion, patients treated with an antibiotic were more likely to get cured than patients on placebo. The overall cure rate was 67% for amoxicillin, 64% for amoxicillin - clavulanate and 43% for placebo.
Pulmoclear
It contains a combination of two medicines, Acebrophylline and Acetylcysteine. They belong to the class of bronchodilators and mucolytics, respectively. Pulmoclear works by relaxing the airways and loosening the cough, thus making the expulsion of cough easy.
Indications :
Pulmoclear Tablet is used for relieving the symptoms of coughing, wheezing, congestion and blockage in the airways in copd.
3) What could be the causes for her current acute exacerbation?
Ans :
- The pt. was started on antitubercular drugs even though she was tested negative for AFB. ATT includes drugs like ISONIAZIDE , RIFAMPACIN , ETHAMBUTOL , PYRAZINAMIDE AND STREPTOMYCIN .
- ISONIAZIDE can cause side effect like hypersensitivity reaction. COPD is a also an allergic which might have exacerbated due to use of isoniazide.
• Exacerbation can also be due to right heart failure.
4) Could the ATT have affected her symptoms? If so how?
Ans : YES, some drugs like isoniazide could could acute exacerbation of COPD thereby increasing the symptoms
5)What could be the causes for her electrolyte imbalance?
Ans :
- Electrolyte imbalance is found among people with Copd, especially for people who are female, 60+ old, take medication Spiriva and have High blood pressure.( this pt. is also hypertensive).
- Patients with COPD tend to retain sodium. In addition, serum potassium should be monitored carefully, because diuretics, beta-adrenergic agonists, and theophylline act to lower potassium levels.
- Beta-adrenergic agonists also increase renal excretion of serum calcium and magnesium, which may be important in the presence of hypokalemia.
- Activation of the renin-angiotensin-aldosterone system and inappropriately elevated plasma arginine vasopressin in COPD may aggravate the electrolyte imbalance during acute exacerbation of COPD.
• In this case patient is also treated with ATT which are nephrotoxic which can also cause electrolyte imbalance.
NEUROLOGY
CASE 1
A 40 Year Old Male with Complaints of Irrelevant Talking
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans :
- The patient is a chronic alcoholic, he drinks about 3-4quarters/day. He had developed seizures following the cessation of alcohol for 24hours it is due to the following reason:-alcohol affects the way in which nerve cells communicate. receptors are specialized proteins on the surface of nerve cells that receive chemical signals from one another. With long-term alcohol consumption, receptors affected by alcohol undergo adaptive changes in an attempt to maintain normal function.
- Two important brain communication systems affected by alcohol involve the neurotransmitters: gamma-aminobutyric acid and glutamate.
GABA is an inhibitory neurotransmitter that helps to regulate brain function by rendering nerve cells less sensitive to further signaling. single doses of alcohol facilitate the inhibitory function of the GABA receptor, contributing to alcohol intoxicating effects. During withdrawal, brain GABA levels fall below normal and GABA activity declines. The combination of reduced brain GABA levels and GABA a receptor sensitivity may be contributed an adaptation to the presence of alcohol. In the absence of alcohol, the resulting decrease in inhibitory function may contribute to Symptoms of nervous system hyperactivity associated with both acute and protracted AW.
The major excitatory neurotransmitter in the brain is glutamate, which communicates with three major subtypes of glutamate receptors. Among these, the N-methyl-D-aspartate (NMDA) receptor plays a role in memory, learning, and the generation of seizures. Alcohol inhibits the excitatory function of the NMDA receptor in laboratory studies at concentrations associated with mild to moderate alcohol intoxication in humans. As with the increased inhibitory function of the GABAA receptor, the decreased excitatory function of the NMDA receptor is consistent with alcohol’s general sedative effect. Long-term alcohol administration produces an adaptive increase in the function of NMDA receptors. Acute AW activates glutamate systems. In turn, AW seizures are associated with increased NMDA receptor function. Persistent alterations in NMDA receptor function may potentiate the neurotoxic and seizure-inducing effects of increased glutamate release during withdrawal.
- The symptom: irrelevant talking, decreased food intake, tremors, sleep disturbance is due to the following reason: chronic alcohol consumption causes thiamine deficiency due to impaired absorption of thiamine from the intestine, a possible genetic predisposition, inadequate diet, reduced storage of thiamine in the liver and other nutritional deficiencies.
Thiamine, one of the first B vitamins to be discovered also known as Vitamin B1, is a coenzyme that is essential for intricate organic pathways and plays a central role in cerebral metabolism. This vitamin acts as a cofactor for several enzymes in the Krebs cycle and the pentose phosphate pathway, including alpha-keto-glutamic acid oxidation and pyruvate decarboxylation. Thiamine-dependent enzymes function as a connection between glycolytic and citric acid cycles. Therefore, deficiency of thiamine will lead to decreased levels of alpha-keto-glutarate , acetate, citrate, acetylcholine and accumulation of lactate and pyruvate. This deficiency can cause metabolic imbalances leading to neurologic complications including neuronal cell death. Neuronal death in the mammillary bodies and thalamus were implicated in multiple cases of Wernicke encephalopathy studied. Studies involving computed tomography (CT) and magnetic resonance imaging (MRI) of patients with Wernicke encephalopathy revealed lesions in the thalamus with dilated ventricles and volume loss in the mammillary bodies. The lesions are usually symmetrical in the midbrain, hypothalamus, and cerebellum.
The kidneys have an important job as a filter for harmful substances .alcohol causes changes in the function of the kidneys and makes them less able to filter the blood .alcohol also affects the ability to regulate fluid and electrolytes in the body. In addition, alcohol can disrupt hormones that disrupt hormones that affect kidney function .people who drink too much are more likely to have high blood pressure. High blood pressure is a common cause of kidney disease. The increase in levels of urea, creatinine, uric acid leads to uraemic encephalopathy. which causes asterixis.
- The deficiency of thiamine and increase in levels of toxins in the body due to renal disease is the primary etiology of the patient's problem.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANS:
I) Thiamine helps the body cells change carbohydrates into energy. It has been used as a supplement to cope with thiamine deficiency.
ii)Lorazepam binds to benzodiazepine receptors on the postsynaptic GABA-A ligand-gated chloride channel neuron at several sites within the central nervous system.it enhances the inhibitory effects of GABA, which increases the conductance of chloride ions into the cell.
iii)pregabalin subtly reduces the synaptic release of several neurotransmitters, apparently by binding to alpha2-delta subunits, and possibly accounting for its actions in vivo to reduce neuronal excitability and seizures.
iv)Lactulose is used in preventing and treating clinical portal-systemic encephalopathy. Its chief mechanism of action is by decreasing the intestinal production and absorption of ammonia.
v) Potchlor liquid is used to treat low levels of potassium in the body.
3)Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
Ans : Due to excess thiamine deficiency and excess toxins accumulation due to renal disease caused by excess alcohol addiction.
4) What is the reason for giving thiamine in this patient?
Ans : Chronic alcohol consumption causes thiamine deficiency due to impaired absorption of thiamine from the intestine, Thiamine, one of the first B vitamins to be discovered also known as Vitamin B1, is a coenzyme that is essential for intricate organic pathways and plays a central role in cerebral metabolism. This vitamin acts as a cofactor for several enzymes in the Krebs cycle and the pentose phosphate pathway, including alpha-keto-glutamic acid oxidation and pyruvate decarboxylation. Thiamine-dependent enzymes function as a connection between glycolytic and citric acid cycles. Therefore, deficiency of thiamine will lead to decreased levels of alpha-keto-glutarate, acetate, citrate, acetylcholine, and accumulation of lactate and pyruvate. This deficiency can cause metabolic imbalances leading to neurologic complications including neuronal cell death.
5) What is the probable reason for kidney injury in this patient?
Ans : The kidneys have an important job as a filter for harmful substances .alcohol causes changes in the function of the kidneys and makes them less able to filter the blood .alcohol also affects the ability to regulate fluid and electrolytes in the body. In addition, alcohol can disrupt hormones that disrupt hormones that affect kidney function .people who drink too much are more likely to have high blood pressure. High blood pressure is a common cause of kidney disease.
6) What is the probable cause for the normocytic anemia?
Ans : Heavy alcohol consumption can cause generalized suppression of blood cell production and the production of structurally abnormal blood cell precursors that cannot mature into functional cells. Alcoholics frequently have defective red blood cells that are destroyed prematurely, possibly resulting in anemia(which is normocytic normochromic)
7) Could chronic alcoholism have aggravated the foot ulcer formation? If yes, how and why?
Ans : The pt. is already diabetic and therefore formation of foot ulcer is high(macrovascular complication).In a patient of chronic alcoholic the immune system is weak due to the affect on blood cells formation and iron absorption, therefore , due to this healing of an ulcer dampens.
CASE 2
A 52 year old male with Cerebellar Ataxia
https://kausalyavarma.blogspot.com/2021/05/a-52-year-old-male-with-cerebellar.html?m=1
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans : Evolution of symptomatology:
- 7days back- H/O giddness with one episode of vomiting
- 4days back- H/O consumption of alcohol , following giddness and postural instability
- 4days back-Associated with bilateral hearing loss, aural fullness, presence of tinnitus
- 4 days back- associated with vomiting 2-3 episodes.
- presents with slurring of speech, and deviation of mouth.
Anatomical location- There is a presence of an infarct in the inferior cerebellar hemisphere of the brain.
Etiology- Ataxia is the lack of muscle control or co-ordination of voluntary movements, such as walking or picking up objects. This is usually a result of damage to the cerebellum (part of the brain that controls muscle co-ordination)
Many conditions cause cerebellar ataxia- Head trauma, Alcohol abuse, certain medications eg. Barbituates, stroke, tumours, cerebral palsy, brain degeneration etc.
In this case, the patient has hypertension for which he has been prescribed medication that he has not taken. Stroke due to an infarct can be caused by blockade or bleeding in the brain due to which blood supply to the brain is decreased, depriving it of essential oxygen and nutrients. This process could’ve caused the infarct formation in the cerebellar region of the brain, thus causing cerebellar ataxia.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Ans :
- Tab Vertin 8mg- This is betahistine, which is an anti- vertigo medication
- MOA- It is a weak agonist on H1 receptors located on blood vessels of the inner ear. This leads to local vasodilation and increased vessel permeability. This can reverse the underlying problem.
- Indications- Prescribed for balance disorders. In this case it is used due to patients history of giddiness and balance issues.
- Tab Zofer 4mg- This is ondanseteron. It is an anti emetic
- MOA- It is a 5H3 receptor antagonist on vagal afferents in the gut and they block receptors even in the CTZ and solitary tract nucleus.
- Indications- Used to control the episodes of vomiting and nausea in this patient.
- Tab Ecosprin 75mg- This is aspirin. It is an NSAID
- MOA- They inhibit COX-1 and COX-2 thus decreasing the prostaglandin level and thromboxane synthesis
- Indications- They are anti platelet medications and in this case used to prevent formation of blood clots in blood vessels and prevent stroke.
- Tab Atorvostatin 40mg- This is a statin
- MOA- It is an HMG CoA reductase inhibitor and thus inhibits the rate limiting step in cholesterol biosynthesis. It decreases blood LDL and VLDL, decreases cholesterol synthesis, thus increasing LDL receptors in liver and increasing LDL uptake and degeneration. Hence plasma LDL level decreases.
- Indications- Used to treat primary hyperlipidemias. In this case it is used for primary prevention of stroke.
- Clopidogrel 75mg- It is an antiplatelet medication
- MOA- It inhibits ADP mediated platelet aggregation by blocking P2Y12 receptor on the platelets.
- Indications- In this case it decreases the risk of heart disease and stroke by preventing clotting
- Thiamine- It is vitamin B1
- It is naturally found in many foods in the human diet. In this case, the patient consumes excess alcohol- so he may get thiamine deficiency due to poor nutrition and lack of essential vitamins due to impaired ability of the body to absorb these vitamins.
- Indications- Given to this patient mainly to prevent Wernickes encephalopathy- that can lead to confusion, ataxia and opthalmoplegia.
- Tab MVT- This is methylcobalamin
- Mainly given in this case for vitamin B12 deficiency.y.
3) Did the patients history of denovo HTN contribute to his current condition?
Ans : A cerebellar infarct is usually caused by a blood clot obstructing blood flow to the cerebellum. High blood pressure that is seen in hypertension (especially if left untreated) can be a major risk factor for the formation of cerebellar infarcts.
Increased shear stress is caused on the blood vessels. The usual adaptive responses are impaired in this case, thus leading to endothelial dysfunction in this case. High BP can also promote cerebral small vessel disease. All these factors contribute to eventually lead to stroke.
4) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic type of stroke?
Ans : Atrial fibrillation and alcohol Drinking excessive amounts of alcohol can trigger atrial fibrillation – a type of irregular heartbeat. Atrial fibrillation increases your risk of stroke by five times, because it can cause blood clots to form in the heart. If these clots move up into the brain, it can lead to stroke.
CASE 3
A 45 Years old female patient with palpitations, pedal edema, chest pain, chest heaviness, radiating pain along left upper limb.
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans : Evolution of symptomatology :
- 10 years ago- had an episode of paralysis attack on all four limbs( due to hypokalemia)
- 8 month ago- B/L pedal edema
- 7months ago- had blood infection
- 2months back- neck pain--diagnosed with cervical spondylosis
- 6days ago- left upper limb pain associated with tingling and numbness
- 5days ago- chest pain , palpitations and SOB
Anatomical localization according to present symptomology is Heart.
Primary etiology of the pt. problem of palpitation , chest pain and SOB is HYPOKALEMIA and for radiating pain of left upper limb is CERIVAL SPONDYLOSIS.
2) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
Ans : The pt. is suffering with HYPOKALEMIC PERIODIC PARALYSIS.
Hypokalemic periodic paralysis (hypoKPP), also known as familial hypokalemic periodic paralysis (FHPP),[1] is a rare, autosomal dominant channelopathy characterized by muscle weakness or paralysis when there is a fall in potassium levels in the blood. In individuals with this mutation, attacks sometimes begin in adolescence and most commonly occur with individual triggers such as rest after strenuous exercise (attacks during exercise are rare), high carbohydrate meals, meals with high sodium content, sudden changes in temperature, and even excitement, noise, flashing lights, cold temperatures and stress. Weakness may be mild and limited to certain muscle groups, or more severe full-body paralysis. During an attack, reflexes may be decreased or absent. Attacks may last for a few hours or persist for several days. Recovery is usually sudden when it occurs, due to release of potassium from swollen muscles as they recover. Some patients may fall into an abortive attack or develop chronic muscle weakness later in life. Current risk factor : due to use of diuretics.
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
Ans : Changes seen in ecg
Earliest changes : decreased T- wave amplitude, ST depression, prolonged PR interval, presence of U waves, T- wave inversion or flat.
In severe cases - ventricular fibrillation, rarely AV block
Symptoms of hypokalemia
Weakness and fatigue, palpitations, muscle cramps and pain, anxiety, psychosis, depression, delirium.
CASE 4
55years old patient with seizures.
1.Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
Ans :
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
Ans :
First the pt. did not have LOC which might mean the pt. has focal seizer which could most commonly can be simple partial A/K/A focal seizers without impairment of awareness that is without LOC . Then the pt. has developed generalized tonic clonic seizers which is usually associated with LOC.
CASE 5
A 48 year old male with seizures and altered sensorium
1) What could have been the reason for this patient to develop ataxia in the past 1 year?
Ans :
- This pt. is a chronic alcoholic who drinks few bottles per day which might have lead to multiple falls causing minor head injuries which he has always neglected and has not got it treated.
- These minor injuries must have been in cerebellar regions which over time lead to edema and damage and caused change in gait ( ataxia type of gait).
- Traumatic brain injury is a common cause of cerebellar damage. This type of injury is usually caused by situations such as automobile accidents, work injuries, or intentional blunt force trauma to the head. Some of the most frequently reported symptoms of damage to the cerebellum include slurred speech, loss of balance, and a lack of coordination.
2) What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses ?
Ans :
- Analyses demonstrated an association of rare and moderate alcohol consumption with decreased risk of both lobar and nonlobar ICH. Heavy alcohol consumption demonstrated a strong association with increased nonlobar ICH risk.
- Study demonstrated potential protective effects of rare and moderate alcohol consumption on ICH risk. Heavy alcohol consumption was associated with increased ICH risk. Race/ethnicity was a significant factor in alcohol-associated ICH risk; heavy alcohol consumption in black and Hispanic participants poses significant nonlobar ICH risk.
• Chronic alcoholism can impair synthetic function of liver causing coagulopathy leading to intra cranial bleed.
CASE 6
A 30 year old male patient with weakness of right upper limb and lower limb
1.Does the patient's history of road traffic accident have any role in his present condition?
Ans :
The RTA may have caused an internal brain injury or injury to any vessel which lead to ischemia which was left undiagnosed nd in mean time due to hypoxia turned into infarct.
there is also another possibility , that is RTA leading to brain injury which was treated at that time but incompletely . over time edema must have occurred or rupture of vessel due to any pressure effect leading to stroke.
2.What are warning signs of CVA?
Ans : • sudden numbness or weakness in the face, arm or leg especially on one side of the body.
•sudden confusion ,trouble speaking or difficulty understanding speech .
• sudden trouble seeing in one or both the eyes.
•sudden trouble walking ,dizziness, loss of balance or lack of co ordination
•sudden severe headache with no known cause.
If you think someone may be having a stroke , act FAST and do the following simple test :
F - FACE : Ask the person to smile. Does one side of the face droop ?
A - ARMS : Ask the person to raise both arms .
S - SPEECH : Ask the person to repeat a simple phrase. Is the speech slurred or strange ?
T - TIME : If you see any of these immediately reach hospital.
3.What is the drug rationale in CVA?
Ans :
Mannitol
Because of its osmotic effect, mannitol is assumed to decrease cerebral edema. Mannitol might improve cerebral perfusion by decreasing viscosity and as a free radical scavenger, it might act as a neuroprotectant.
Ecospirin
For the prevention of heart attack, stroke, heart conditions such as stable or unstable angina due to a blood clot.
Atorvastatin
It is used to lower cholesterol and reduce risk of heart diseases.
RT feed
Nursing procedure to provide nutrition to those people who are either unable to obtain nutrition by mouth or are not in a state to swallow food safely.
4. Does alcohol has any role in his attack?
Ans :
Alcohol increases the risk of hemorrhagic stroke.
A hemorrhagic stroke occurs either when an
aneurysm bursts, or a weakened blood vessel leaks. The result is bleeding either inside the brain, causing an intracerebral hemorrhage, or, less commonly, bleeding between the brain and the tissue covering it, causing a so-called subarachnoid hemorrhage.
The adverse effect of alcohol consumption on
blood pressure – a major risk factor for stroke – may increase the risk of hemorrhagic stroke .
5.Does his lipid profile has any role for his attack?
Ans : The lipid profile of the pt. is almost normal except HDLP which is little less. This pt. is neither hypertensive nor diabetic , so lipid profile having any role in attack is unlikely here.
But in general, Low HDL, High Homocysteine Predicts Poor Stroke Recovery For Diabetics. Patients with diabetes and low levels of HDL cholesterol, and high levels of homocysteine who have had a mild to moderate ischemic stroke were twice as likely as their counterparts without these conditions to have poorer cognitive function and greater disability after a stroke.
CASE 7
A 50 year old patient with cervical myelopathy.
1)What is myelopathy hand ?
Ans : Myelopathy hand is characterized by muscle wasting and motor dysfunction with cervical spondylosis. This is termed as " Amyotrophic type of myelopathy hand ". The main clinical features are localized wasting and weakness of extrinsic and intrinsic muscles of hand but not accompanied by either sensory loss or spastic quadriparesis.
2)What is finger escape ?
Ans : It is described by Ono as one of the signs of cervical cord damage .
It is deficient adduction and or extension of the ulnar 2-3 digits. It must be differentiated from similar looking signs affecting little finger include Wartenberg's sign and Digit quinti sign. To differentiate from these we need to look for other signs of cervical myelopathy.
3)What is Hoffman’s reflex?
Ans : It is neurological examination finding elicited by a reflex test which can help verify the presence or absence of issues arising from the corticospinal tract. A positive hoffman's reflex indicates an upper motor neuron lesion and corticospinal pathway dysfunction likely due to cervical cord compression.
CASE 8
17 year old female with seizures
1) What can be the cause of her condition?
Ans : It might be cortical venous thrombosis according to the the results of imaging.
2) What are the risk factors for cortical vein thrombosis?
Ans : Infections:
1.Meningitis, otitis,mastoiditis
2.Prothrombotic states:
3.Pregnancy, puerperium,antithrombin deficiency protein c and protein s deficiency,Hormone replacement therapy.
Mechanical:
1.Head trauma,lumbar puncture
2.Inflammatory:
3.SLE,sarcoidosis,Inflammatory bowel disease.
4.Malignancy.
5.Dehydration
6.Nephrotic syndrome
Drugs:
1.Oral contraceptives,steroids,Inhibitors of angiogenesis
2.Chemotherapy:Cyclosporine and l asparginase
Hematological:
1.Myeloproliferative Malignancies
2.Primary and secondary polycythemia
Intracranial :
1.Dural fistula,
2.venous anomalies
Vasculitis:
1.Behcets disease wegeners granulomatosis
3)There was seizure free period in between but again sudden episode of GTCS why? resolved spontaneously why?
Ans : Seizures are resolved and seizure free period got achieved after medical intervention but sudden episode of seizure was may be due to any persistence of excitable foci by abnormal firing of neurons.
4) What drug was used in suspicion of cortical venous sinus thrombosis?
Ans :
Anticoagulants are used for the prevention of harmful blood clots.
Clexane ( enoxaparin) low molecular weight heparin binds and potentiates antithrombin three a serine protease Inhibitor to form complex and irreversibly inactivates factor xa.
CARDIOLOGY
CASE 1
A 78 year old male with shortness of breath, chest pain , bilateral pedal edema and facial puffiness.
1.What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
Ans : The amount of blood pumped out of the heart with each beat is called the ejection fraction (EF). A normal EF is usually around 55 to 70 percent, but it can be lessened in some forms of heart failure.
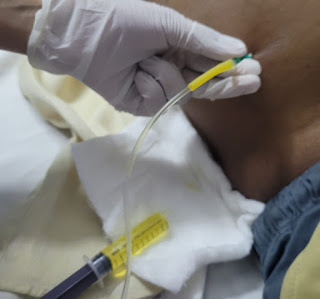
2) Why haven't we done pericardiocentesis in this patient?
Ans: Pericardiocentesis is performed for medical patients either as therapeutic or diagnostic procedure. it is indicated when acute or chronic pericardial effusion causes cardiac tamponade. It is done when pericardial effusion is not resolving on its own. In this patient ,as the fluid which has accumulated was resolving on its own pericardiocentesis is not required. At the time of admission it was 2.07cms and at the time of discharge it was 1.4mm.
3.What are the risk factors for development of heart failure in the patient?
Ans: NON- RISK FACTORS
*Age
*Gender
MODIFIABLE RISK FACTORS
* Hypertension
*Smoking
*Type 2 diabetes
* Kidney disease
OTHER GENERALIZED RISK FACTORS
* Obesity and overweight
* Physical inactivity
*Heredity
*High blood cholesterol
* Stress
*Alcohol
4.What could be the cause for hypotension in this patient?
Ans: The patient was anemic with Hb of 8gm/dl. One of the severe complication of anemia is tissue hypoxia which further lead to hypotension.
CASE 2
A 73 year old male patient with pedal edema, shortness of breath and decreased urine output.
1.What are the possible causes for heart failure in this patient?
Ans : * Obesity
* Alcohol
* Diabetes mellitus
* Hypertension
2.what is the reason for anemia in this case?
Ans : In this patient the cause of anemia can be due to alcohol. Alcohol can impact RBC production as it decreases the number of precursor cells to be made.In addition to this, alcohol can also impact RBC maturation causing abnormality or dysfunction of cells. When enlarged RBC ( due to alcohol ) are produced, as a complication, they are likely to be destroyed faster than normal cells.
Alcohol may also affect how nutrients are absorbed from the food. Alcohol induced malnutrition tends to lead to iron and folic acid deficiency which are needed for the proper formation of hemoglobin.
3.What is the reason for blebs and non healing ulcer in the legs of this patient?
Ans : This patient had recurrent blebs and ulcer on lower limbs. this can be due to Type 2 diabetes mellitus .
Ulcers in people with diabetes are most commonly caused by :
* Poor circulation
* High blood sugar
* Nerve damage
* Irritated or wounded feet
Nerve damage is a long term effect and can lead to a loss of feeling in feet. Nerve damage reduces sensitivity to foot pain and results in painless wounds that can cause ulcers. When ulcers occur in these patients , they have delayed healing due to poor circulation and high glucose levels as the infection fighting capacity is impaired.
4. What sequence of stages of diabetes has been noted in this patient?
Ans :
alcohol------obesity------impaired glucose tolerance------diabetes mellitus------microvascular complications like retinopathy and diabetic foot ulcer-------macrovascular complications like coronary artery disease , coronary vascular disease and peripheral vascular disease.
CASE 3
Atrial fibrillation and Biatrial Thrombus in a 52yr old Male
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans :Evolution of symptomatology and event timeline -
Past-
10yrs ago - Operation for Hernia
Since 2-3 yrs - Facial puffiness
1 yr ago - SOB grade II
1 yr ago - was diagnosed with Hypertension.
When the patient came to OPD -
Since 2 days - SOB which progressed from Grade II to Grade IV.
Since 2 days - Decreased urine output.
Since 1 day - Anuria
After admission -
CT scan - Showed dilated pulmonarypulmonary vessels and thrombi in the atria.
2D Echo - Showed LV dysfunction.
Anatomical location - Atria (SA node)
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Ans :
- Digoxin - It is a cardiac glycoside
MOA - It increases intracellular sodium that will cause an influx of calcium in the heart and cause an increase in contractility. It is vagomimetic.
Indications - Heart failure and arrhythmias.
- Carvediol - It is a beta-blocker.
MOA - It blocks the beta receptors and lowers the heart rate, blood pressure and strain on the heart.
Indications - Hypertension, heart failure, LV dysfunction with MI.
- Heparin - It is an anti-coagulant
MOA - It produces its major anticoagulant effect by inactivating thrombin and activated factor X through an antithrombin dependent mechanism. By inactivating thrombin, heparin not only prevents fibrin formation but also inhibits thrombin induced activation of platelets and of factors V and VIII.
Indications - Prophylaxis and treatment of venous thromboembolism and pulmonary embolism; Atrial fibrillation with embolization ; chronic consumptive coagulopathies.
- Acitrom - It is an Oral anti-coagulant
MOA - It inhibits the reduction of Vitamin K by Vitamin K reductase. This prevents carboxylation of Vitamin K dependent clotting factors, II, VII, IX, X and interferes with coagulation.
Indications - Thromboembolic diseases such as DVT, Coronary occlusion
- Cardivas - It is an adrenergic blocker
MOA - Reversibly binds to beta adrenergic receptors on cardiac myocytes. Inhibition of these receptors prevent a response to the sympathetic nervous system, leading to decreased Heart rate and contractility
Indications - Hypertension, Angina and heart failure..
• Dytor - It is a diuretic. Contains Torsemide +spironolactone
MOA - Through its action in antogonizing effect of Aldosterone, spironolactone inhibits the exchange of sodium for potassium in the distal renal tubule and helps to prevent potassium loss.
Indications - Edema, Hypertension.
- Taxim - It is a cephalosporin antibiotic.
MOA - It is bactericidal through inhibition of cell wall synthesis.
Indications - Treatment of infections of throat, airway and urinary tract ; Typhoid fever.
- Thiamine - It is Vitamin B1.
MOA - Rapid restoration of Thiamine levels
Indications - Wernicke's encephalopathy, infantile beriberi etc.
- Inj. HAI - It is a short acting insulin.
3) What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
This patient is having type 4 CRS.
4) What are the risk factors for atherosclerosis in this patient?
Ans :
HTN, physical inactivity and obesity in this pt.
5) Why was the patient asked to get those APTT, INR tests for review?
Ans :
Anticoagulants being given to patient , therefore CVA and for predicting future ischemic attacks we do the above tests.
CASE 4
67 year old patient with acute coronary syndrome
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans : Evolution of symptomatology :
- 12yrs ago- diagnosed with DM.
- 1yr ago - has heartburn like symptoms which are relieved without medication
- 7months ago- diagnosed with TB nd took treatment
- 6months ago- diagnosed with HTN
- 1/2 hour back- SOB grade 4
Anatomical localization in this patient is Heart.primary etiology is partial blockage in coronary artery.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Ans : Metaprolol
3) What are the indications and contraindications for PCI?
Ans : INDICATIONS:
Acute ST-elevation myocardial infarction (STEMI)Non–ST-elevation acute coronary syndrome (NSTE-ACS)Unstable angina.Stable angina.Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)High risk stress test findings. CONTRAINDICATIONS:
Intolerance for oral antiplatelets long-term.Absence of cardiac surgery backup.Hypercoagulable state.High-grade chronic kidney disease.Chronic total occlusion of SVG.An artery with a diameter of <1.5 mm.
4) What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on overtesting and overtreatment important to current healthcare systems?
Ans : when PCI is performed in pt. who does not need it ..it lead to complications.
Economy, Planet, Security, World and Health. But an epidemic of overtreatment — too many scans, too many blood tests, too many procedures — is costing the nation’s health care system at least $210 billion a year, according to the Institute of Medicine, and taking a human toll in pain, emotional suffering, severe complications and even death.
CASE 5
A 60 year old male patient with chest pain, giddiness and sweating.
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans :
Evolution of symptomatolgy:
- 8yrs back- diagnosed with DM
- 3 days back- developed chest pain radiating to back and dragging type
- since morning - giddiness and profuse sweating.
Anatomical localization in this pt. is heartprimary etiology is uncontrolled DM nd inferior wall MI
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Ans :
TAB. ASPIRIN 325 mg PO/STAT
MOA : It is a cox inhibitor which inhibits prostaglandin formation which prevents inflammation, swelling and pain.
INDICATIONS : Fever, relieve mild to moderate pain
TAB ATORVAS 80mg PO/STAT
MOA : It is a HMG CoA reductase inhibitor. It inhibits conversion of HMG CoA to mevalonic acid.
INDICATIONS : High cholesterol, lower risk of heart attack and stroke, in coronary heart disease.
TAB CLOPIBB 300mg PO/STAT
INJ HAI 6U/IV STAT
It is a short acting insulin.
3) Did the secondary PTCA do any good to the patient or was it unnecessary?
Ans : starting PTCA after 12 hours is acceptable but after 3 days is not correct and can lead to complications.
CASE 6
A case of cardiogenic shock
1. How did the patient get relieved from his shortness of breath after i.v fluids administration by rural medical practitioner?
Ans :
2. What is the rationale of using torsemide in this patient?
Ans : Torsemide is a diuretic used to treat high blood pressure and condition of excess fluid retention in the body due to heart failure. This will help to relieve his symptom of SOB.
3. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
Ans : The antibiotic was administered to treat the UTI as the patient did complain of whitish discharge in the urine which may be a sign of infection. The patient also has a risk for further infection as he is using a Foley's catheter. So the antibiotic can be prophylactic too.
GASTROENTEROLOGY AND PULMONOLOGY
CASE 1
A 33 year old man with pancreatitis , pseudocyst and left broncho - pleural fistula.
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans :
- 5years ago- developed pain abdomen and vomiting
- 1 year back - Vomitings
- 1 week ago- developed pain abdomen
- 4days ago- developed fever , constipation and burning micturition.
Anatomical localization in the patient is Pancreas. Primary etiology of the condition is chronic alcohol intake.
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
Ans :
- drugs used are meropenem , metrogyl , amikacin , octreotide and thiamine.
- Here all three of these (Inj. Meropenem, Inj. Metrogyl, Inj. Amikacin ) are used as antibiotics to control infection and ; to prevent septic complications of acute pancreatitis.
- ING. OCTREOTIDE 100 mg SC , BD
* It is a Somatostatin long acting analogue.
* It is used here to decrease exocrine secretion of pancreas and it also has anti- inflammatory & cytoprotective effects.
- ING. THIAMINE 100 mg in 100 ml NS IV , TID
* It is B1 supplement.
* It is given here because; due to long fasting & TPN usage , body may develop B1 deficiency
* Wernicke encephalopathy secondary to B1 deficiency may be caused... so a prophylactic B1 supplemention is necessary.
*It is opiod analgesic used for pain relief.
CASE 2
25 year old male with epigastric pain.
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
Ans : Pleural effusion is cause for patient's dyspnoea. Pleural effusion may occur due to pancreaticopleural fistula secondary to leak and disruption of pancreatic duct.
2) Name possible reasons why the patient has developed a state of hyperglycemia.
Ans :
- Pancreatitis is nothing but the inflammation of the pancreas. Acute pancreatitis is caused when such an inflammation of the pancreas comes all of a sudden and brings the acute amount of pain.
- Pancreas that is mainly responsible for the production of the hormone, insulin. However, when the organ gets inflammation due to various reasons, the cells in the pancreas that are responsible for the production of the hormone are damaged. Thus, diabetes is caused. Thus, as a result of pancreatitis, a patient will require administering insulin through various external sources. The most common form of diabetes that is mainly known to be caused as a result of the pancreatitis is known as secondary diabetes.
3) What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
Ans :
- The liver is one of the largest and most complex organs in the body. It is the chief organ responsible for metabolizing alcohol and is especially vulnerable to alcohol related injuries.
- As alcohol is broken down inside the liver, it releases a number of potentially dangerous byproducts that may damage the liver more than the alcohol itself
- Each of these toxins plays a role in the damage of the liver and the subsequent release of enzymes from the cells
- Heavy drinking for as little as just a few days can lead to fatty liver, the earliest stages of alcoholic liver disease
4) What is the line of treatment in this patient?
CASE 3
45 year old male patient with fever, pain abdomen, decreased urine output and abdominal distension.
1) what is the most probable diagnosis in this patient?
Ans : The most probable diagnosis is Ruptured liver abscess and hemoperitoneum. This will give reasoning to the abdominal distension and blood which is aspirated.
2) What was the cause of her death?
Ans : There is no true inflammation. Here sudden rupture of an amoebic liver abscess into the pericardium may result in a very severe shock and death within hours. Such cases can present with sudden retrosternal pain and shock with a previous history of epigastric pain and fever of few days' duration.
3) Does her NSAID abuse have something to do with her condition? How?
Ans : drug induced hepatitis.
Drug-induced hepatitis is a redness and swelling (inflammation) of the liver. It is a rare condition caused by harmful (toxic) amounts of certain medicines, vitamins, herbal remedies, or food supplements.
NSAIDS are associated with hepatic side effects ranging from asymptomatic elevations in serum aminotransferase levels and hepatitis with jaundice to fulminant liver failure and death.
NEPHROLOGY AND UROLOGY
CASE 1
Post TURP with non oliguria ATN diabetic nephropathy
1. What could be the reason for his SOB ?
Ans :
- Being short of breath can be related to the kidneys in two ways. First, extra fluid in the body can build up in the lungs. And second, anemia (a shortage of oxygen-carrying red blood cells) can leave your body oxygen-starved and short of breath.
- can it be because of dehydration as the pt. used diuretics ?
- here I am assuming kidney failure lead to diastolic dysfunction which lead to pulmonary congestion leading to SOB.
2. Why does he have intermittent episodes of drowsiness ?
Ans : A decrease in the renal clearance of waste nitrogenous products accompanies with their continuous generation leads to diverse uremic retention products such as urea, creatinine, guanidine and homocysteine. Many of these toxins affect functioning of cells and organs, resulting in endothelial vascular injury, neurotoxicity and cognitive dysfunction.
3. Why did he complaint of fleshy mass like passage in his urine?
Ans :
The fleshy mass like passage in his urine might be due to excessive pus cells in the urine (according to the reports) and the frothy appearance may be due to the presence of proteins. The urine is pale yellow in colour.
4. What are the complications of TURP that he may have had?
Ans :
- A complication of TURP that the patient may have had is 'TURP syndrome'.
- It is rare but is life threatening.
- Cause- It may occur as a consequence of absorption of fluids used to irrigate the bladder during the operation.
- Signs and symptoms are due to fluid overload and electrolyte disturbances and hyponatremia.
CASE 2
An Eight year old with Frequent Urination
1.Why is the child excessively hyperactive without much of social etiquettes ?
Ans : One possible Provisional diagnosis of this patient is ADHD (Attention deficit/Hyperactive disorder).
Symptoms may start before the age of 12 and include inattention and hyper active impulsive behavior.
Inattention -
They have trouble to stay focused in tasks or play.
They appear not to listen even when spoken directly.
They are easily distracted.
They avoid or dislike tasks that require mental effort.
Hyper active impulsive -
Have difficulty sitting in one place and are always on the run.
Fidget with their hands or legs.
Talk too much
Have difficulty waiting for their turn.
Academic difficulties are frequent as are problems with relationships.
2. Why doesn't the child have the excessive urge of urination at night time ?
Ans : It maybe Psychosomatic. The child has the urge to urinate in the morning due to stress or mental conflict. During sleep, the kid is free of stress and may not have the urge to urinate excessively.
3. How would you want to manage the patient to relieve him of his symptoms?
Ans : The only management is reassurance to the kid and his relaxation by reducing stress. The problem will resolve overtime (most commonly by the time he reaches 10yrs).
There are a variety of psychotherapeutic approaches employed by psychologists and psychiatrists; the one used depends on the patient and the patient's symptoms. The approaches include psychotherapy, cognitive-behavior therapy, support groups, parent training, meditation, and social skills training.
INFECTIOUS DISEASES
A 40 year old female with dysphagia, fever and cough.
1.Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
Ans :
- Clinical history- weight loss, recurrent chest infections, trauma, malignancy or ingestion of caustic substances, pyrexia of unknown origin
- Physical findings- Uncontrolled coughing after swallowing, often worse with carbonated drinks (ONO sign).
2) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
INFECTIOUS DISEASES AND
HEPATOLOGY
CASE 1
A 55 year old male patient with pain abdomen decreased appetite and fever .
1. Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors
present in it ? What could be the cause in this patient ?
Ans : Here in this case , drinking locally made alcohol can be a cause of liver abscess due to predisposing factors present in it.
2. What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
Ans : Liver abscess can be pyogenic or amoebic. Alcohol can predispose to liver abscess through a multitude of mechanisms , including hepatic damage by alcohol ,lowered body resistance and suppression of liver function due to poor nutritional status of habitual consumers of alcohol, increased presence of pathogen in the liquor prepared locally with poor regard to aseptic procedures and depression of immune mechanisms in chronic alcoholics. Alcohol induced hepatic dysfunction and possible suppression of amoebistatic immune mechanisms by substances in the beverages could also attributed in the mechanism. It is noted that alcoholics had larger abscesses ,a greater frequency of complications and delayed resolution of abscesses.
3. Is liver abscess more common in right lobe ?
Ans : Left lobe of liver receives blood from
- Inferior mesenteric artery
- Splenic veins
Right lobe of liver receives blood from
- Superior mesenteric artery
- Portal veins
Streaming effect in portal circulation is the causative factor for liver abscess being more common in right lobe.
4.What are the indications for ultrasound guided aspiration of liver abscess ?
Ans : Aspiration of abscess is rarely needed
•with large abscess
•those who appear to superinfected
•large abscess having impending rupture Or compression sign
•thin rim of liver tissue around the abscess ( < 10mm )
•sero negative abscess
•failure in the improvement following non invasive treatment after 4 to 5 days
CASE 2
A 25 year old male patient with abdominal pain and fever.
1) Cause of liver abcess in this patient ?
Ans : Cause of liver abscess may be due to contamination of food/ fluid history which is not mentioned. Malnutrition and poor personal hygiene are also risk factors for liver abscess . The cause of abscess in this patient is infection with entamoeba leading to liver abscess.
2) How do you approach this patient ?
Ans : In clinical practice we treat both pyogenic and amoebic liver abscess empirically. So we cover both bacterial causes with broad spectrum antibiotics and also amoebic cause mostly with metronidazole. Next we administer patient with analgesic and antipyretic such as Dolo and Ultracet tablets to relieve pain and fever. Abscess and may get ruptured if untreated and can cause peritonitis and shock.
3) Why do we treat here ; both amoebic and pyogenic liver abcess?
Ans : we treat both pyogenic and amoebic liver abscess empirically because we cant differentiate whether the abscess is because of bacterial infection or amoebic infection.
So we cover both bacterial causes with broad spectrum antibiotics and also amoebic causes mostly with metronidazole.
4) Is there a way to confirm the definitive diagnosis in this patient?
Ans :
Based on right hypochondriac and epigastric pain , fever
USG finding of hyperechoic mass in right lobe of liver along with other supportive investigations like leucocytosis (suggestive of infection/inflammation) and ALP ( Alkaline phosphatase ) rise in LFT is a suggestive diagnosis of LIVER Abscess.
* Considering the following factors:
1) Age of the patient (21) - young & gender- male
2) Single abscess,
3) Right lobe involvement,
# The abscess is most likely to be AMOEBIC LIVER Abscess.
We can also do USG guided aspiration to confirm the definitive diagnosis in this patient and also the stool culture.
INFECTIOUS DISEASES ( MUCORMYCOSIS, OPHTHALMOLOGY, OTORHINOLOGY AND NEUROLOGY)
CASE 1
50 year old male with altered sensorium
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans : 3 years ago - hypertension was diagnosed
10 days ago - fever with chills and rigor
4 days ago - facial puffiness and peri orbital edema
4 days ago - weakness of right upper and lower limb
Anatomical localization of the problem is Oral cavity, nose and eye.
Primary etiology : It can be considered as diabetes as DKA is the most important risk factor for mucormycosis.
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
Ans : here drugs used in this patient are
* Itraconazole
* Deoxycholate amphotericin B
* Inj. liposomal amphotericin B
3) What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
Ans : The surge in apparent rise of mucormycosis has been attributed to improper use of steroids to treat covid 19 patients coupled with poorly managed diabetes. In addition , India has an epidemic of type 2 diabetes and significant proportion of patients with diabetes are diagnosed late in the illness.this can also be the contributing factor.
INFECTIOUS DISEASES ( COVID - 19 )
for this question that contains details of many of our covid 19 patients documented over this month and we would like you to:
1) Sort out these detailed patient case report logs into a single web page as a master chart
2) In the master chart classify the patient case report logs into mild, moderate severe and
3) indicate for each patient, the day of covid when their severity changed from moderate to severe or vice versa recognized primarily through increasing or decreasing oxygen requirements
4) Indicate the sequence of specific terminal events for those who died with severe covid (for example, altered sensorium, hypotension etc).
Medical Education
Experiential learning is a very important method of Medical education and while the E logs of the students in the questions above represent partly their and their patient's experiences, reflective logging of one's own experiences is a vital tool toward competency development in medical education and research. A sample answer to this last assignment around sharing your experience log of the month can be seen in the link below but while this is by a student onsite in hospital and not locked down at home we would be very interested to learn about your telemedical learning experiences from our hospital as well as community patients over the last month even while locked down at home:
Making this elogs gives us a great
opportunity to enhance our knowledge. At
the same time it is giving us a chance to open up with our friends in order to discuss the cases and interact with the faculty. In these difficult times teleconsultation helped us a lot to add up to our existing knowledge and skills.































































Comments
Post a Comment