N.Deepa, 8th semester
Roll no. 93
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Following is the view of my case :
( date of admission :18/10/2021 )
( history taken on : 19/10/2021 )
CASE :
A 43 year old male was brought to the casuality with chief complaints of involuntary movements in the right upper and lower limb.
HOPI :
He is a 43 yr old male born out of a non -consanguinous marriage. Patient had weakness in the fingers of right limb since childhood and he carry out his daily activities with his left hand. 5 years ago patient had angry burst out and used to beat his family members . He was taken to a hospital where they prescribed him antipsychotics. Tab. Risperidone 2mg twice daily and Tab. Trihexiphenidryl 2mg once daily. Since then patient is continuously on antipsychotics and there are no episodes of anger burst out.
Patient had fever spikes on 17/10/2021. On 18/10/21 post lunch around 4 pm patient had involuntary movements of right upper and lower limb for 10 minutes.There was loss of consciousness.No deviation of mouth. No urinary or fecal incontinence after seizure. He was taken to a hospital. During the journey patient had 2 episodes of seizures each lasting for around 2-3 minutes in the span of 1 hour. He also had a episode of vomiting.
PAST HISTORY :
There is no history of seizures in the past.
No history of HTN, DM, TB, Asthma.
No surgical history
PERSONAL HISTORY :
Diet : Mixed
Appetite : Normal
Sleep : Disturbed sleep before antipsychotics. Now it is adequate
Bowel and bladder habits : Regular
Addictions : Alcohol occasionally
Allergies : No food and drug allergies
FAMILY HISTORY :
No history of seizures in the family.
No history of psychiatric problems in the family.
GENERAL EXAMINATION :
The patient was not conscious.
moderately built and well nourished.
Pallor- Absent
Icterus- Absent
Clubbing- Absent
Cyanosis- Absent
Lymphedenopathy- Absent
Edema- Absent
VITALS-
Temperature- febrile
BP- 140/90 mm of hg
Pulse- 83 bpm
Respiratory Rate- 18
Oxygen saturation- 98% on room air
SYSTEMIC EXAMINATION :
CNS :
Gcs - E2 V1 M3
Higher mental functions - cannot be elicited
Cranial nerve examination
• optic nerve -
• trigeminal nerve -
• facial nerve -
• glossopharyngeal nerve -
• hypoglossal nerve -
Motor examination :
Right Left
TONE
Upper limb hypotonia hypotonia
Lower limb hypotonia hypotonia
POWER
Upper limb 0/5 0/5
Lower limb 0/5 0/5
REFLEXES
Biceps + +
Triceps - -
Supinator - -
Knee + +
Ankle + +
Plantar - -
Gait cannot be examined.
Sensory system cannot be examined.
Cvs : S1 S2 heart sounds heard, No murmurs
Respiratory system : Bilateral air entry present.
Abdomen : Soft and non - tender. Bowel sounds are heard. No organomegaly.
DIFFERENTIAL DIAGNOSIS :
• Meningitis
• Left hemiparesis
• Neuroleptic malignant syndrome
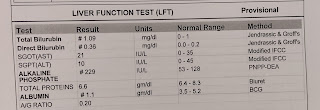
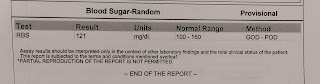
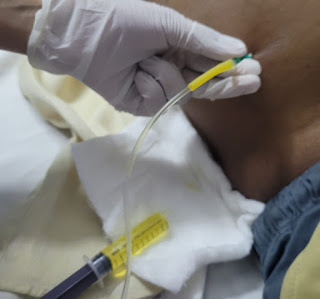
INVESTIGATIONS :
ECG :
MRI VENOGRAM:
In the patient MRI was done on 18th and 19th. After MRI patient had episode of vomiting.
PSYCHIATRIC REFERAL :
OPHTHALMOLOGY REFERAL :
DIAGNOSIS :
Focal seizures ( Rt side ) with secondary generalisation
TREATMENT :
On 19/10/2021
• Inj. MANNITOL 100 ml/IV / TID
• Inj. LEVIPIL 1 gm / IV / BD
• Inj. LORAZEPAM 2cc / IV / SOS
• Stop antipsychotics
• RT feeds
- 50ml water 2 hourly
- 100ml milk 4 hourly
• Inj. MONOCEF 1g / IV / BD
• Inj. ENOXAPARIN 40mg every 12 hourly















Comments
Post a Comment