48 year old male with abdominal distension
Dr.N.Deepa , Internee
Roll no. 105
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Date of admission : 19/04/2023
CASE :
A 48 year old male, auto driver by occupation came to the opd with chief complaints of
- Abdominal distension since 20 days
- Bilateral pedal edema since 15 days
- Decreased urine output since 10 days
- Shortness of breath since 10 days
-Blood in stools since 5 days
- Loose stools since 4 days
HOPI :
Patient ws apparently normal 20 days back.Then he developed abdominal distension which was insidious in onset and gradually progressed to present size.
No complaints of pain abdomen.
He developed bilateral pedal edema since 15 days which is pitting type and extending till the knee joint.
He has decreased urine output since 10 days.
No complaints of burning micturition.
History of shortness of breath since 10 days, insidious in onset, gradually progressed from grade 1 to grade 3 .SOB increased on exertion and relieved on taking rest.No orthopnea .No PND.
He gave history of blood in stools since 5 days -- blood at the end of defecation.
Not associated with pain ,no mass per rectum.
History of loose stools since 4 days,4-5 episodes per day.
No history of fever, vomiting,chest pain,giddiness.
PAST HISTORY :
History of jaundice in the past- 2 years back and 6 months back and was managed conservatively with medication.
K/c/o Hypertension since 10 years, initially was on T.TELMA 80 mg which was later reduced to T.TELMA 40 mg and now the patient is on T.AMLONG 5mg + ATENOLOL 50mg PO OD
N/k/c/o DM-2,TB,CAD,CVD
PERSONAL HISTORY :
Diet : Mixed
Appetite : Decreased since 20 days
Bowel and bladder movements : Decreased urine output
Sleep : Adequate
No allergies
He is alcoholic since 25 years.
FAMILY HISTORY :
No history of diabetes or hypertension in the family.
GENERAL EXAMINATION :
Patient is examined in a well lit room after taking the consent.
He is conscious, coherent and cooperative.
Well oriented to time, place and person.
Pallor - absent
Icterus - present
Cyanosis - absent
Clubbing - absent
Generalized Lymphadenopathy - absent
Bilateral pedal edema - present
Pitting edema extending till the knee joint.
VITALS :
Pulse - 76 beats per minute, regular in rhythm, normal in volume and character of vessel, no radio- radial delay, no radio - femoral delay.
Respiratory rate - 20 cycles per minute
Blood pressure - 110/70 mm of hg, measured in the left arm in supine position
Temperature - afebrile
Spo2 - 98% at room air
GRBS - 94 mg/dL
SYSTEMIC EXAMINATION :
CVS :
S1 S2 heard, no murmurs
CNS :
No neurological deficit
RS :
Bilateral air entry present,no adventitious sounds.
ABDOMINAL EXAMINATION :
Inspection - abdomen distended
Umbilicus is flat and central
No visible scars or sinuses
No visible gastric peristalsis
Palpation - No local rise of temperature
No tenderness
Organs couldn't be palpated
Percussion - fluid thrill present
Auscultation - bowel sounds normal
INVESTIGATIONS :
Investigations sent on 19/4/2023
2D echo
Ultrasound abdomen:
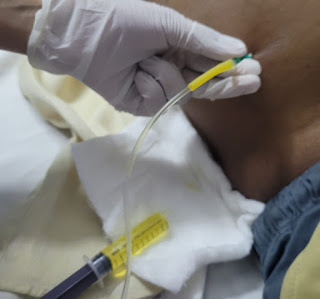
Ascitic tap was done ( diagnostic and therapeutic tap)
DIAGNOSIS :
•DECOMPENSATED CHRONIC LIVER DISEASE
•INTERNAL HAEMORRHOIDS SECONDARY TO PORTAL HTN
• GRADE 4 OESOPHAGEAL VARICES
TREATMENT :
Day 1 (19/4/2023):
• Inj.THIAMINE 200mg in 100ml NS IV OD
• Tab.UDILIV 300mg PO BD
•Tab.ALDACTONE 50mg PO OD
• Inj.PAN 40 mg IV OD
• Tab.SPOROLAC DS PO TID
• ORS sachets - 2 sachets in 1 litre of water and 200ml after each episode
• Protein powder in a glass of milk
• Monitor vitals,input and output, Abdominal girth.
Diagnostic and therapeutic tap was done and around 800ml of ascitic fluid was drawn.
Day 2 (20/4/2023) :
Loose stools subsided
Abdominal girth 102cm -------99cm
Weight 70kgs -----69kgs
Psychiatry referal was done i/v/o alcohol dependence
Patient is psychoeducated and Tab.Pregabalin 75 mg is advised.
Surgery referral done i/v/o blood in stools
and the patient is diagnosed to have internal haemorrhoids secondary to portal hypertension,advised banding or sclerotherapy if bleed continues or if there is significant drop in haemoglobin.
• Inj.THIAMINE 200mg in 100ml NS IV OD
•Tab.UDILIV 300mg PO BD
•Tab.ALDACTONE 50mg PO OD
• Inj.PAN 40 mg IV OD
• Tab.PREGABALIN M 75mg PO HS
•Protein powder 2tbsp in a glass of milk
• Monitor vitals,input and output, Abdominal girth.
• Restriction of fluids <1.5lit/day
Day 3 ( 21/4/2023) :
Endoscopy was done and diagnosed to grade 4 oesophageal varices
•Tab.UDILIV 300mg PO BD
•Tab.ALDACTONE 50mg PO OD
• Inj.PAN 40 mg IV OD
• Tab.PREGABALIN M 75mg PO HS
•Protein powder 2tbsp in a glass of milk
• Monitor vitals,input and output, Abdominal girth.
• Restriction of fluids <1.5lit/day
Therapeutic ascitic tap was done and around 500ml of fluid was drawn.
Day 4 (22/4/2023):
• Inj.NORAD 4mg in 46ml NS @4ml/hr
• Tab.UDILIV 300mg PO BD
•Tab.ALDACTONE 50mg PO OD
• Inj.PAN 40 mg IV OD
• Tab.PREGABALIN M 75mg PO HS
•Protein powder 2tbsp in a glass of milk
• Monitor vitals,input and output, Abdominal girth.
• Restriction of fluids <1.5lit/day
























Comments
Post a Comment