26year old male with pyrexia under evaluation
Dr.N.Deepa , Internee
CASE :
Patient was brought to the opd with chief complaints of
Fever since 1week
c/o generalised weakness and headache since 1 week
c/o vomitings since 3 days
c/o loose stools since 3 days
HISTORY OF PRESENT ILLNESS:
Patient was apparently alright 1week ago then he developed fever which is high grade, intermittent, associated with chills and rigor.
He was in Orissa while he developed fever then he returned to his home 2 days later.
He also had headache and general weakness
He developed vomitings since 3 days, 5 episodes, with food as content, non bilious, non projectile, not blood stained
Loose stools since 3 days, 3 episodes/day, watery, green coloured, not blood stained.
He went to a doctor outside but the symptoms did not subside, then he came here to our hospital.
INVESTIGATIONS:
DIAGNOSIS:
Pyrexia under evaluation - Dengue
- Clinical malaria
With AKI (resolved),ALI (resolving) with HEPATOSPLENOMEGALY with BICYTOPENIA
TREATMENT:
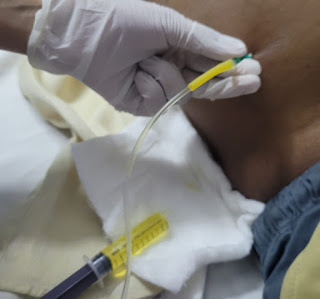
1.I.V fluids NS, RL, DNS@100ml/hr
2.Inj DOXY 100mg IV/BD
3.Inj. PAN 40mg IV/OD
4.INJ. NEOMOL 1gm I.V/sos if temp >102°f
5.Tab. DOLO 650mg po tid
6.Inj. ZOFER 4MG IV/TID
7.Syp. CREMAFFIN 15ML PO/BD
8.Monitor vitals
9.Strict I/O Charting
10.Protein rich diet
2 FFP transfusion were done in view of coagulation derangement but it was followed by reaction.The patient developed sudden excessive sneezing,cough with expectoration,high grade fever with drop in oxygen saturation. On auscultating,he had wheeze.
He is then treated with inj.AVIL , Inj.HYDROCORT and nebulizations.
The patient is now subjectively feeling better.




Comments
Post a Comment